Common HPB Conditions
Patient Information
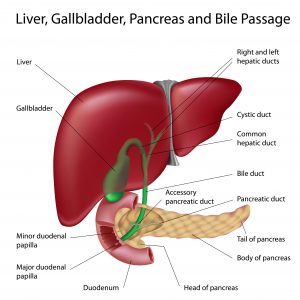
Liver
Liver Cancer
• The most common primary cancer affecting the liver, almost 8 out of every 100 000 Australians will develop this disease
• The incidence of this cancer has been steadily rising in Australia over the last 30 years due to both better detection methods, and the rise of chronic liver disease (= cirrhosis)
What are the risk-factors for liver cancer?
• Liver cancer most often occurs in the context of cirrhosis
• Cirrhosis is irreversible liver damage (often described as scarring) caused by chronic insult to the liver by another disease-process such as:
o Hepatitis B infection
o Hepatitis C infection
o Chronic excessive alcohol intake
o Fatty liver disease (= non-alcoholic steatohepatitis)
o Iron overload (= hemochromatosis)
• A minority of patients will develop liver cancer without significant liver disease
How is liver cancer diagnosed?
• Many patients with known risk-factors for liver cancer are in surveillance programs
• Some patients may be diagnosed both with cirrhosis and liver cancer at the same time
• Other patients may be diagnosed following imaging to investigate blood test abnormalities, or to investigate for other diseases (such as gallstones)
How is liver cancer treated?
• Many treatments exist for liver cancer, with the type of treatment dependent on both the stage of the liver cancer and the degree of liver disease (= cirrhosis) affecting the patient
• Treatments that can cure liver cancer include:
o Resection of the tumour as part of a partial liver resection
o Resection of the tumour as part of a liver transplant
o Burning the tumour in the liver (= ablation)
• Treatments that can slow the progression of liver cancer include:
o Injection of chemotherapy into the arteries of the liver supplying the tumour (= transarterial chemoembolization or TACE)
o Injection of radiation treatment into the tumour (= selective internal radiation therapy or SIRT)
o Newer chemotherapy agents
Colorectal cancer liver metastases
• Colorectal cancer liver metastases refers to the spread of bowel cancer to the liver
• More than half of patients diagnosed with bowel cancer will have spread to the liver at some point
How are colorectal cancer liver metastases diagnosed?
• Some patients are diagnosed at the time of their bowel cancer diagnosis (= synchronous disease)
• Others are diagnosed on surveillance after they undergo surgery to remove the primary bowel cancer (= metachronous disease)
How are colorectal cancer liver metastases treated?
• It has been well-proven that successful removal of all metastatic colorectal cancer deposits to the liver prolongs survival
o Most often this involves surgical resection of a portion or multiple portions of the liver to ensure all the cancer is removed
o It is important however to ensure that once all the deposits have been removed that enough liver is left for the patient to survive
• Sometimes other procedures might be completed to improve the likelihood of all the cancer deposits being removed, these include:
o Removing the main blood supply to one part of the liver in order that another part grows so that a more extensive liver resection can be undertaken to remove all the cancer deposits (= portal vein embolization)
o A 2-stage approach (that is, resect deposits in one part of the liver at one time, and then return and remove the remaining deposits at another time, often after the remaining liver has been allowed to grow)
o Burning of one or multiple cancer deposits (= ablation)
• Because liver metastases may return at any point following liver resection to remove them, some patients may have multiple liver surgeries to remove different deposits over the course of their lifetime
Benign growths and diseases of the liver
Liver cysts
o A collection of fluid lined by cells of the liver that can range from almost undetectable to larger than the liver itself
o The vast majority are asymptomatic and do not require treatment
o Complications of cysts are more common in very large cysts and include:
– Pain from pressure on the outside of the liver, known as the capsule
– Bleeding into the cyst
– Infection in the cyst
o Complicated cysts may be treated with surgical drainage
Liver haemangioma
o The most common benign lesion (= tumour) of the liver
o Often diagnosed incidentally on imaging of the liver for another reason
o Almost universally require no specific treatment
Focal Nodular hyperplasia
o A benign lesion of the liver caused by abnormal growth of liver cells surrounding unusual blood vessels within the liver
o Much more common in women
o Does not require any further treatment once confidentally diagnosed on liver imaging
Liver adenoma
o An uncommon benign lesion of the liver, with some sub-types associated with developing liver cancer (= HCC)
o 11 times more common in women compared to men, with 90% of women diagnosed having current or previous use of the oral contraceptive pill
o May be treated with cessation of the oral contraceptive pill, whilst other patients may require ongoing surveillance imaging to ensure the lesion does not grow
o Some patients require resection of their lesion(s) including those >5cm in size, those affecting men, and any that are causing complications such as bleeding
Hydatid cyst
o An uncommon infection of the liver caused by a parasitic worm called Echinoccus
o Typically affects farm-workers, often amongst Australian migrant populations
o Treated with a combination of antibiotics for the infection (called albendazole) and either surgical cyst drainage or resection
Liver abscess
o An infection of the liver associated with a collection of pus
o Most commonly caused by bacteria from other abdominal infections being transported to the liver via its blood supply, or via infection of a blocked bile duct (= cholangitis) tracking into the liver
o Although less uncommon in Australia, liver abscess can also be caused by a parasite called Entamoeba
o Patients with liver abscess may be very unwell with sepsis due to the infection
o Treated with a combination of antibiotics for the infection and drainage of the collection of pus
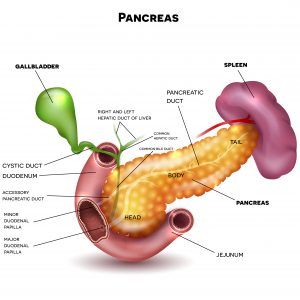
Pancreas
Pancreatic Cancer
• Although pancreatic cancer is the 8th most commonly diagnosed cancer in Australia, it is 3rd most common cause of cancer death
• Despite significant advances worldwide in pancreatic cancer management over the last 10 years, only ~1 in 8 patients will remain alive 5 years after their initial diagnosis
What are the risk-factors for pancreatic cancer?
• Age – More common in patients over 60
• Smoking – At least 2-3-fold increased risk
• Obesity/metabolic syndrome – Almost doubles the risk
• Family history
o If you have 2 first-degree relatives who have had pancreatic cancer, this increases your individual risk by 15 times
o Also associated with certain inherited (= hereditary) conditions
• Importantly however, many patients diagnosed with pancreatic cancer have no recognisable risk-factors
How is pancreatic cancer diagnosed?
• Pancreas cancer can grow silently and the symptoms may be non-specific including upper abdominal pain, weight loss, or loss of appetite
• Unexpected development of adult-onset diabetes, or deterioration in blood sugar control in an established diabetic may be indirect evidence of pancreatic cancer
• Cancers of the pancreas located near the liver may cause blockage of the bile duct leading to darkening of the urine, pale stools, and yellowing of the skin and eyes (= jaundice)
• Many patients are diagnosed due to a suspicious lesion being shown on an imaging investigation
How is pancreatic cancer treated?
• The only proven way to potentially cure pancreatic cancer is to remove the tumour surgically and then complete a 6-month course of chemotherapy postoperatively
• Depending on what part of the pancreas is involved, surgery may require removal of part of the pancreas along with the bile duct and duodenum (known as a Whipple procedure), or removal of the end part of the pancreas along with the spleen (known as a radical distal pancreatectomy & splenectomy)
• Unfortunately, even with successful surgery and chemotherapy, pancreatic cancer is difficult to cure and many patients will ultimately die from their disease
Acute Pancreatitis
• An acute inflammatory process of the pancreas characterised by the sudden onset of abdominal pain and the presence of raised levels of pancreatic digestive enzymes in the bloodstream due to activation of the digestion properties of the pancreas within the organ itself
• This condition is very common in Australia due to the significant presence of both gallstones and alcohol misuse in our population
Why does acute pancreatitis occur?
• The pancreas is an important organ that serves two major functions:
o The control of sugar in our blood via release of insulin
o Digestion of nutrition via release of certain enzymes into the digestive tract
• From an insult to the pancreas. Pancreatitis occurs when the enzymes of digestion are inappropriately activated within the pancreas rather than in the digestive tract
o The body recognises this as being abnormal and mounts an inflammatory response against the pancreas in an attempt to turn off the activation
o Unfortunately, this response can itself cause more problems, including compromising the blood supply to the pancreas
o A complex interplay of reactions can then occur which ultimately put the viability of the pancreas at risk, and potentially make the patient very unwell
• Most patients with pancreatitis will be unwell in hospital for a few days and then improve independent of any specific treatment
o A minority will develop life-threatening complications and may require extended periods being cared for in intensive care
• The most common causes of pancreatitis are gallstones and excessive alcohol intake
o Other causes include:
– Very high blood fat levels (= hypertriglyceridaemia)
– Very high blood calcium level (= hypercalcaemia)
– An endoscopic procedure used to access the bile duct (= ERCP)
– Certain medications
– Certain viral infections
– Activation of the patient’s own immune system against the pancreas (= autoimmune pancreatitis)
How is acute pancreatitis treated?
• For many patients, no specific treatment is required the body recovers on its own
• Further management is focussed on preventing another episode of pancreatitis, this may mean you’re recommended to have your gallbladder removed (=laparoscopic cholecystectomy), or advised to abstain from insults such as alcohol or certain medications
• Rarely other surgical or endoscopy procedures are required, though these normally occur as part of a complicated admission to hospital for severe forms of the disease
Pancreatic cysts
Many different growths can occur on the pancreas that contain fluid (= cysts)
Serous cystic neoplasm
• A completely benign cystic growth that most often occurs in the head of the pancreas. Does not require consideration for resection or further surveillance.
Mucinous cystic neoplasm
• The most common cystic growth, with women 20 times more likely to have this develop compared to men
• Considered a pre-malignant lesion. The patient will usually be recommended to undergo surgical resection of the growth
Intraductal papillary mucinous neoplasm (= IPMN)
• A growth that occurs in the duct system of the pancreas which causes a blockage.
• These growths produce a substance called mucin which can lead to blockage
• Depending on the appearance of these growths on scans, you may be recommended to undergo surgery.
Pseudocyst
• Pseudocysts are caused by severe episodes of pancreatitis allowing fluid to leak from the pancreas which is then trapped within scar tissue outside the pancreas.
• Pseudocysts only require treatment if they are causing problems such as infection, blockage of the stomach, or blockage of the bile duct
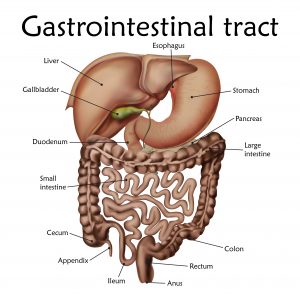
Gallbladder
Gallstones
• Approximately 1 in 5 Australians will be diagnosed with gallstones in their lifetime
• The majority of people who have gallstones don’t know they have them
• The older you get, the more likely you are to be diagnosed with gallstones
• Patients with gallstones causing problems should be considered for a laparoscopic cholecystectomy
What are the risk-factors for gallstones?
• Cholesterol stones (= 90% of patients)
o Largely a result of oversecretion of cholesterol in bile
– Age
– Female sex hormones
• Female gender
• Oral contraceptives
• Pregnancy
– Obesity & metabolic syndrome
– Rapid weight reduction
– Hyperlipidaemia syndromes
– Hereditary factors
• Pigment stones
o Mainly a result of the increased breakdown in blood products (= haemolysis)
– Cirrhosis of the liver
– Chronic haemolytic syndromes
– Biliary infection
– Gastrointestinal disorders
• Crohn’s disease
• Ileal resection or bypass
• Cystic fibrosis with pancreatic insufficiency
What problems do gallstones cause?
• Biliary colic
o Temporary obstruction of bile outflow from the gallbladder by gallstones
o Causes gallbladder spasm and severe but episodic pain typically associated with meals, especially those with a higher fat content
• Acute cholecystitis
o Impaction of gallstones in the outflow tract of the gallbladder leads to definitive obstruction of and rising pressure within the gallbladder body
o The ensuing inflammatory process may lead to:
– Swelling of the gallbladder
– Compromised blood flow (= ischaemia) to the gallbladder
– Infection within the gallbladder
– Perforation of the gallbladder
• Pancreatitis
o Acute inflammatory condition of the pancreas that varies in its clinical course from mild to life-threatening
• Bile duct stones (= choledocholithiasis)
o Gallstones can pass from the gallbladder to the bile duct which connects the liver to the bowel
o Stones in the bile duct may lead to:
– Obstruction of the bile duct (a leading cause of jaundice)
– Infection of the bile duct (a potentially life-threatening issue)
– Infection of the liver (a potential cause for liver abscess)
How are gallstones treated?
• Unlike kidney stones, there is no procedure to remove gallstones and leave the gallbladder within the body
• Most commonly gallstones are treated with key-hole surgery to remove the gallbladder (= laparoscopic cholecystectomy)
o Rarely, the gallbladder will not be able to be removed with key-hole surgery and open surgery will be required
• Some patients may require another endoscopy procedure (= ERCP) to remove bile duct stones (= choledocholithiasis)
• Rarely, some patients will require surgery on their bile duct (= choledochotomy) to remove bile duct stones. Often this can be completed with key-hole surgery
Gallbladder cancer
• An uncommon cancer in Australia affecting ~2 out of every 100 000 people. Women are 3 times more likely to be afflicted compared to men
What are the risk-factors for gallbladder cancer?
• Age – More common in patients aged over 60
• Gallstones – Effectively every patient with gallbladder cancer has gallstones. However, the vast majority of patients with gallstones will NEVER develop gallbladder cancer
• Gallbladder polyps
• Background – More common in patients of Pakistani, native American, or Chilean ethnicity
How is gallbladder cancer diagnosed?
• Most patients will be diagnosed after their cancer is discovered unexpectedly following removal of their gallbladder for other reasons (usually for gallstone-related symptoms)
• Some patients may be having surveillance of a previously diagnosed gallbladder polyp
• More advanced forms of the disease may be diagnosed following investigations for abdominal pain, lethargy, loss of appetite, weight loss, or jaundice
How is gallbladder cancer treated?
• Some people diagnosed unexpectedly will not require further treatment
• Others will require further surgery after their initial gallbladder removal to remove associated lymph nodes and a small portion of the liver normally attached to the gallbladder as a way of knowing whether the cancer has been completely removed
• Rarely, patients with gallbladder cancer are diagnosed following suspicious imaging and proceed straight to a radical operation to remove the gallbladder, lymph nodes, and part of the liver all at once. This may be done with key-hole surgery.
Gallbladder polyps
• Small abnormal outgrowths of tissue from the internal wall of the gallbladder most commonly diagnosed incidentally on ultrasound
Why are they a problem?
• There is an association between true gallbladder polyps (knowns as adenomas) and gallbladder cancer
• Interestingly, although people may have surgery for gallbladder polyps, many are found to have other benign disease processes masquerading as true polyps once their surgery is complete
o These includes cholesterol deposits (= cholesterolosis), abnormal thickening of the gallbladder wall (= adenomyomatosis), or scarring of the inner lining of the gallbladder (= inflammatory pseudopolyps)
o None of these conditions have any association with gallbladder cancer
How are gallbladder polyps treated?
• Because of the risk with some gallbladder polyps harbouring gallbladder cancer, certain patients with the disease will be recommended for surgery to remove the gallbladder including:
o Any polyp measuring more than 10mm in size
o Any polyp thought to be causing symptoms (although this is uncommon)
• Many patients will not require surgery for gallbladder polyps, however, they may require surveillance to make sure the polyp is not growing
Bile duct cancer
• An uncommon cancer in Australia affecting 1-2 in every 100 000 patients
• Bile duct cancer is further defined by what part of the bile duct is primarily affected:
o Bile ducts inside the liver (=intrahepatic cholangiocarcinoma)
o Bile ducts at the border of the inside and outside of the liver (= hilar cholangiocarcinoma or Klatskin’s tumours)
o Bile ducts outside the liver (= extrahepatic cholangiocarcinoma)
What are the risk-factors for bile duct cancer?
• Age – More common in patients over 60
• Background – More common in patients of south-east Asian ethnicity
• Certain other conditions affecting the bile ducts
o Primary sclerosing cholangitis
o Recurrent pyogenic cholangiohepatitis
o Choledochal malformations
o Infection with parasitic worms within the bile duct and/or liver (= liver flukes)
How is bile duct cancer diagnosed?
• This can be dependent on the position of tumour
• Extrahepatic and Hilar cholangiocarcinoma are more likely to cause blockage of the bile duct leading to darkening of the urine, pale stools, and yellowing of the skin and eyes
• Intrahepatic cholangiocacinoma may grow silently and may present with non-descript symptoms such as abdominal pain, weight loss, or lethargy
• Any of these cancers may be diagnosed after an imaging investigation undertaken for other reasons
How are bile duct cancers treated?
• The only way to potentially cure bile duct cancer is to remove the tumour surgically. Depending on where the tumour is located this may require resection of part of the liver, resection of part of the bile duct, resection of parts of both these structures, or removal of the bile duct along with part of the pancreas (known as a Whipple procedure)
• Unfortunately, even with successful surgery, bile duct cancer is difficult to cure and many patients will ultimately die from their disease
Professional Affiliations






Book an appointment
I look forward to discussing all aspects of your general surgical care in the future.
